Conversations around fertility and family planning come up a lot on Elpha: from questions about fertility benefits at work to the “best” age for having kids to hiring a surrogate , family planning can be a complicated topic, especially for those who are invested in their work.
Whether you’re just starting to think about your fertility, or you’ve already decided that you want to freeze your eggs or go through IVF treatment, we want to make sure you have access to the resources and support that will help you plan accordingly.
We teamed up with the doctors at Spring Fertility *, a best-in-class fertility center, to answer your questions about fertility, fertility preservation, IVF, and family planning so that you can be empowered with knowledge when evaluating your options.
*Spring Fertility is also offering Elpha members $150 off initial consults in any of their US clinics using the promo code ELPHA (note that this cannot be combined with any insurance).
Keep reading to find the consolidated answers to the Q&A with Spring Fertility Drs. Catha Fischer, Monica Pasternak, and Peter Klatsky which cover:
Fertility preservation options
Embryo freezing vs. egg freezing
Best practices before an embryo transfer
Things to consider if doing a FET abroad
Vetting fertility centers
Pricing and logistics of egg freezing
The “best” age for egg freezing
Egg quality vs. egg quantity
Risks associated with egg age
Miscarriages and age
Other variables and their influence on fertility
Infertility in couples
Effects of COVID on fertility
Endometriosis
Bicornate uterus
Supplementation of DHEA
Fertility after childbirth
Reclaiming your body’s natural cycle postpartum
Multiple cycles of IVF or egg retrievals
Timing between pregnancies after IVF
Fertility preservation options
The uncertainty about outcomes is one of the hardest things for women freezing eggs. Egg freezing was introduced clinically in 2012 (meaning, it was no longer considered experimental), and we are still learning about the success rates. Much of our data comes from women who use frozen donor eggs to achieve healthy pregnancies. Frozen donor eggs have high success rates and function similarly to “fresh” eggs if they survive the freezing process.
Embryo freezing vs. egg freezing
Fertility preservation does not need to be limited to egg freezing.
Embryo freezing is also another option. This is effective (and provides greater certainty than egg freezing) and is ideal for a committed couple that wants to have children together in the future. The benefit of freezing embryos is that you can genetically test embryos to ascertain whether they are chromosomally normal. If you create a chromosomally normal embryo, you can expect an approximately 60-70% chance of a live birth with each genetically “normal” embryo. If you have already identified your life partner (or sperm source), then freezing embryos, instead of eggs, makes sense.
If you freeze eggs, you preserve your opportunity to choose your sperm source later.
The cost of the opportunity to delay committing your eggs to one sperm source is that eggs do not all survive the freezing process. It's appropriate to assume that 10-20% of the eggs frozen, may not survive that process. When we freeze embryos (fertilized eggs), 99% survive.
REMEMBER: Egg freezing is still a manual process and it is arguably the hardest thing we do in the IVF lab, and is the part of the process reserved for our most senior embryologists. There is a lot of variability in outcomes between patients and also between clinics. We recommend doing this process somewhere with extensive experience. Before you choose a fertility clinic you should ask about the clinic’s:
Survival rates of warmed frozen eggs, and
Blastocyst (early stage of an embryo) development rate of those eggs, at your age
Multiple cycles of IVF or egg retrievals
In general, we do not see much risk of multiple cycles of IVF or egg retrievals. There is a small increased risk of borderline ovarian tumors that has been reported in women after undergoing six retrievals, but the absolute increase in this risk remains very low at less than 1%. The timeline between egg retrieval cycles does not increase your risk of adverse outcomes.
Best practices before an embryo transfer
It is a good idea to evaluate the uterine cavity. Leading up to the transfer, it is standard to monitor uterine lining development. How often you go into your clinic will vary across clinics. It will also vary by patient depending on how often blood work is needed. It's always a good idea to ask the clinic how they use bloodwork or your test results. After transfer, some clinics will check hormone levels prior to a pregnancy test, while others won’t. The key here is that you understand what your clinic is doing and you understand why they are doing it.
Things to consider if doing a FET abroad
Before a Frozen embryo transfer (FET), one typically undergoes a saline sonogram to make sure the uterus has no addressable obstacles to implantation. Once we have initial blood work and a saline sonogram, it is possible that a patient on a medicated or “controlled” protocol for a frozen embryo transfer, may only need to visit their clinic for the day of a transfer (if their doctors accept remote monitoring). Every clinic will have different requirements and slightly different protocols, so the time in the country for the transfer might range anywhere from three days to one month.
Vetting fertility centers
Egg retrieval and IVF are sophisticated and challenging services. You want to go to a center that has great physicians, scientists, and outcome data. Sites like FertilityIQ are also great for learning more about other patients’ experiences.
Some questions to consider: who is the provider? Where did they train and practice? What are the success rates of this service? And what are the complication rates? Also, how do they respond to your questions? We feel patients should leave an appointment feeling empowered with more answers. If you are confused after a consultation, maybe it's not a good fit.
Pricing and logistics of egg freezing
Prices vary by clinic and geography (remember cheapest to freeze may not be the cheapest in the long run if the outcomes are worse). The costs of egg freezing vary a bit by region, but in general, the range is $7-15k.
The age at which you decide to freeze your eggs is also a variable to consider when budgeting for fertility treatment. The primary downside to freezing your eggs when you are younger is the annual storage fees, which also vary regionally, but can typically cost from $60 to $100/month.
Eggs, sperm, and embryos do not degrade based on the time that they are cryopreserved. You can store your eggs for as long as you’d like. The primary risks are the momentary process of oocyte cryopreservation and the momentary process of the thaw.
The egg freezing process takes about two weeks. How each woman reacts to egg freezing is different. In general, the more eggs you have growing the more side effects you experience, like bloating. Side effects are reversible and normal. When something increases in size (an ovary), you feel heavier because at that moment you are.
Most of our patients continue to work during the process and may be able to miss only one day of work for the egg retrieval procedure.
The “best” age for egg freezing
Best is a tough word in medicine. A woman’s eggs are highest in quantity and quality when we are young: the quantity of eggs begins to decline in our twenties, the quality of our eggs (meaning, the chance that any one egg can successfully develop into a healthy baby) begins to decline rapidly in our mid to late thirties. In general, there isn’t a dramatic change in either the quantity or quality of eggs until our mid to late thirties.
An important consideration when thinking about fertility preservation is “how likely are you to need to go through IVF in the future.” For example, if a woman knew that she would have to go through IVF, then we would recommend freezing eggs – the younger the better.
For instance, if you know that your fallopian tubes are blocked or damaged, if you have a genetic mutation that you will want to screen for to have a healthy child, or if you have a medical condition that will preclude carrying your own pregnancy (therefore requiring IVF with a gestational carrier), we would recommend freezing eggs as early as possible in order to optimize your chances.
Egg quality vs. egg quantity
The distinction between egg quality and quantity is very important.
Female age is the best predictor of egg quality. Most of the data on using frozen eggs comes from women under 38. Our best understanding of the data is that eggquality, and therefore natural fertility does not decline too much before age 36. We see that eggs frozen after age 35 seem to develop at a lower rate than younger eggs and that those embryos have a higher probability of being abnormal.
The only thing fertility physicians can assess through tests is egg quantity. AMH (Anti Mullerian hormone) count assesses egg quantity and is not a reflection of fertility. Our eggs make AMH at certain stages of their development. Although we have had all our eggs since birth, from our remaining pool of eggs we constantly have new groups being recruited on a cyclic basis throughout our reproductive years.
It's often a good idea to get an initial test of your ovarian reserve with an AMH blood test.
AMH is produced by the groups of eggs that will be recruited and will grow over the next upcoming few months. Hence, a woman with a higher AMH has more eggs being recruited on a month-to-month basis. This most often translates into an ability to produce more eggs if you are going through the IVF or egg-freezing process.
However, it’s important to understand that having a low AMH does not have any relation with your natural fertility.Out of our eggs recruited on a monthly basis, only one (in rare cases, multiple) grows to the point of being released at ovulation and potentially fertilized by sperm. So, the number of eggs that were “contenders” to grow but did not get chosen is really not a predictor of fertility.
Therefore, women with a low AMH can achieve pregnancy as easily as women with a normal or high AMH. But it may mean that their follicle count is lower and that they will produce fewer eggs through the egg freezing or IVF process (if they needed it).
Thus, an initial AMH blood test can be helpful to guide your own timeline in considering egg freezing. This will help you and your physician make a timeline.
(an aside on take-home hormone tests)
There is no take-home test that is as valuable as a consult with a physician. Like everything, it depends on what information you are seeking from these direct-to-consumer tests.
If you want a generalized interpretation of a blood test, these at-home tests are fine. If you are looking for an interpretation that applies to you, then an actual visit to a provider is the best path.
We use AMH as a surrogate marker for the number of eggs we have remaining (higher AMH, more eggs remaining).
It is true that the number of eggs one can obtain declines linearly with age, and this decline begins in ones mid-20s. That said, the decline in number of eggs typically occurs slowly. The average number of eggs retrieved per attempt declines by about 1 egg per year of age.
Helpful data slides that we use from published studies are included below:
Rate of decline in number of usable eggs retrieved per IVF cycle (Attempt):

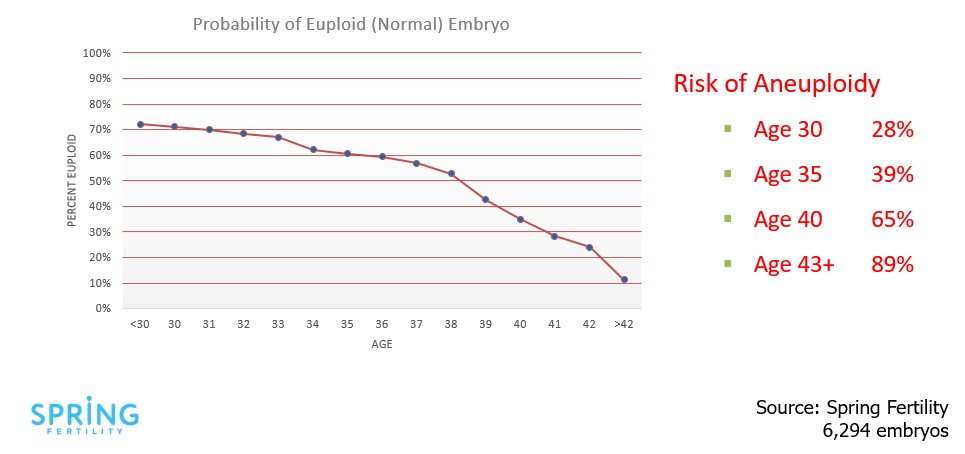
The decline in quality or chance that an embryo has a normal chromosome number over time:
An old study looking at how many eggs were used per live birth at different ages (from 2005-2010 in clinics across Belgium and The Netherlands):

For most women, there is not a big difference in outcome between freezing your eggs at 28 or 34. Every woman should consider her goals with egg freezing and decide when is the best time for her as life events, travel, school, and finances weigh differently for people.
Interestingly, the average age women were freezing their eggs 5 years ago was 37-38. Today, the average age of women freezing their eggs at Spring Fertility is 33.
When considering fertility preservation, one key question we strongly suggest asking yourself is, “how old do I anticipate being when I want to be having my LAST child?”. If the answer to that is over 40, then it may be prudent to learn more about fertility preservation.
Two tools that are helpful as you consider this are an Egg freezing success probability calculator that we created and the Modern Fertility Timeline Tool .
Risks associated with egg age
Eggs that are retrieved from younger women are more likely to produce genetically normal pregnancies. So if you intend to use your eggs to conceive, frozen 36 year old eggs are more likely to develop into healthy pregnancies than older eggs. However, this is in reference primarily to the risk of Downs syndrome, Turner’s syndrome, and miscarriage.
Maternal age is not related to conditions like Autism, schizophrenia or other conditions that are not linked to chromosome number. Interestingly, the man’s age may play a role in the risk of autism, schizophrenia, and neuropsychiatric conditions. So far paternal age has been associated with but is not definitively causal in these conditions. Maternal age or egg age data is centered around genetic abnormalities.
Miscarriages and age
Miscarriages are actually quite common. Approximately 25% of pregnancies will result in a miscarriage at age 35. Six years later, that probability has increased to 50% (at age 41/42). Many times the challenge in having a baby is maintaining the pregnancy.
It's worth seeing a specialist who can evaluate to make sure there are no treatable or diagnosable conditions that put you at higher risk for a miscarriage (eg. a uterine septum, antiphospholipid antibody syndrome, or balanced translocation).
If those tests are negative, there may just be a higher risk due to age. In that case, IVF can help if you test the embryos before putting them back. An embryo with 46 chromosomes would have only a 5-10% risk of miscarriage, regardless of the age of the woman receiving the embryo.
Reducing miscarriage risk via Preimplantation Genetic Testing for Aneuploidy (PGT‐A)
Testing to see if your embryo has 23 pairs of chromosomes (PGT-A) can be helpful in reducing miscarriage risk and reducing the risk of multiple gestations (twins/triplets) by transferring only a single embryo. Like any test, it is important to know that it is not perfect and there is a 4% false-positive rate and a 1-2% chance that after the biopsy, the genetics lab will not be able to determine if the embryo is normal or abnormal. In spite of those recognized limitations, we feel that it is still a helpful test, particularly for women aged 35-42.
PGT-A is meant to assess the genetic composition of embryos and therefore allow physicians to select embryos for transfer. There are many studies showing that embryos are not damaged or harmed by the biopsy; however, the decision about doing PGT-A is individual. In general, we use a woman’s age as a factor in this counseling since, as we get older, our risk of miscarriage or abnormal pregnancies goes up. The decision on if this test is right for you really comes down to individual risk tolerance.
Other variables and their influence on fertility
Infertility in couples
Infertility is diagnosed based on time. About 85% of couples less than 35 years old will achieve a pregnancy within a year. This timeframe changes as we get older because it becomes harder to conceive, so between 36 and 39 we say try for six months before seeking evaluation.
Built into the definition of infertility is the assumption that couples have no issues. If you have irregular cycles or your partner has low sperm counts, then you should seek guidance earlier and potentially before starting.
The idea of an evaluation prior to even trying has merits if you are concerned, but know that these tests are validated, or we know how to interpret them when couples have infertility. In the absence of the diagnosis, when tests return somewhat indeterminate it is challenging to counsel patients on what these mean.
Effects of COVID on fertility
So far, data on covid infection and fertility is reassuring. Having COVID in pregnancy does put you at increased risk of pregnancy loss, so we do encourage everyone to get vaccinated.
Endometriosis
Endometriosis is a condition that affects many different systems. Oftentimes, women with endometriosis have trouble getting pregnant but can achieve a pregnancy with IVF rather than donor eggs or gestational surrogacy. Interestingly, pregnancy actually improves symptoms of endometriosis.
In general, treatment of patients with endometriosis should try to maintain estrogen levels as low as possible to avoid increasing inflammation associated with endometriosis.
Bicornate uterus
It may be worth speaking with a maternal-fetal medicine physician or fertility specialist with the MRI images in order to review your specific situation and risk. From a fertility standpoint, the risks are not around conceiving but more centered on risk of preterm delivery. In general, women with bicornuate uteri have smaller uterine cavities and there is less room for a pregnancy to grow, which can increase the risk of preterm delivery or pregnancy loss.
Supplementation of DHEA
The data around dehydroepiandrosterone (DHEA) are mixed. DHEA is a hormone that helps produce other hormones, including testosterone and estrogen. In general, we do not advise supplementation unless there is a deficiency. These hormones are not static, which is why there are normal ranges. If you are within the normal range, none of us recommend supplementing.
Fertility after childbirth
Reclaiming your body’s natural cycle postpartum
While every woman is different, in general, breastfeeding – particularly if you are feeding many times a day – will suppress your cycle. Remember that the menstrual cycle is set up to achieve a pregnancy, which takes a lot of energy. While your body is expending so much energy to produce milk, it doesn’t have the reserves to support a new pregnancy: so, no cycles. If you scale back on breastfeeding, your cycles should resume.
Timing between pregnancies
There is one study that suggests waiting a year between delivery and any subsequent embryo transfer will be most beneficial (in terms of birth weight and length of gestation). We encourage women to wait at least 10 months from their last delivery and if possible to wait a year before trying to get pregnant again.
We hope you walk away from this resource more informed about fertility, the options that are available for preserving and enhancing it, and what to consider when incorporating family planning into your career.
Every woman and their fertility is different which is why we recommend consulting with a physician about your specific case when evaluating your options.
🥚 Want to consult with the doctors at Spring Fertility ? Use the promo code ELPHA for $150 off initial consults in any of Spring Fertility’s US clinics (note that this cannot be combined with any insurance).
🍼 Looking for a company that will support you as you build your career while you build your family? Check out the Elpha Talent Pool for companies that offer fertility benefits, childcare benefits, 12+ weeks of maternity leave, and more.
🤰 Maybe you want to stay at your company but it doesn’t have a parental leave policy in place. Here’s how one Elpha member secured a maternity leave policy at a company that didn’t have one .






